Connect With Us

Plantar Fibroma
A plantar fibroma is a knot in the arch of the foot. It can cause pain when repeated pressure is applied by walking barefoot or wearing tight shoes. While plantar fibromas can appear in anyone, men who are middle-aged or older are said to be more susceptible. The main symptom of a plantar fibroma is a firm lump on the arch of the foot. If there is pain, it can be intensified by putting pressure on the nodule. The lump can stay one size or grow larger. You may have one or more fibromas in the feet and there tends to be a high incidence of recurring plantar fibromas. Generally, a plantar fibroma can be treated without surgery. Treatment might include steroid injections to help shrink the lump, orthotics to help redistribute weight away from the nodule, plantar fascia stretching, or physical therapy to help use anti-inflammatory medication on the lump. If a lump grows larger or more painful, a podiatrist can be consulted to confirm the diagnosis. The doctor will palpate the lump and this may cause pain that can be felt all the way to the toes. An X-ray, MRI, or biopsy might be done if further evaluation is necessary. A lump in the arch of the foot might be something other than a plantar fibroma, such as cysts, nerve or fatty tumors, swollen tendons, or an infection in the foot. It is important to see a podiatrist for proper diagnosis and treatment of plantar fibromas.
Common Causes of Swollen Ankles
 Ankle swelling, also known as edema, is a familiar condition caused by various factors. The most frequent sources include injuries, such as sprains or fractures, which lead to inflammation and fluid accumulation. Prolonged standing or sitting, especially in hot weather, can also cause swelling due to fluid pooling in the lower extremities. Medical conditions like heart failure, kidney disease, or liver disease can contribute to fluid retention and subsequent swelling. Additionally, chronic venous insufficiency and certain medications, such as those for high blood pressure, can result in ankle swelling. To address ankle swelling, elevate the legs to reduce fluid buildup and improve circulation. Compression socks can help prevent fluid accumulation, while regular movement and exercise promote blood flow. Maintaining a low-sodium diet can also help to manage fluid retention. If you have swelling in your ankles that persists, or that is accompanied by pain, redness, or warmth, it is suggested that you schedule an appointment with a podiatrist for a proper diagnosis and treatment plan.
Ankle swelling, also known as edema, is a familiar condition caused by various factors. The most frequent sources include injuries, such as sprains or fractures, which lead to inflammation and fluid accumulation. Prolonged standing or sitting, especially in hot weather, can also cause swelling due to fluid pooling in the lower extremities. Medical conditions like heart failure, kidney disease, or liver disease can contribute to fluid retention and subsequent swelling. Additionally, chronic venous insufficiency and certain medications, such as those for high blood pressure, can result in ankle swelling. To address ankle swelling, elevate the legs to reduce fluid buildup and improve circulation. Compression socks can help prevent fluid accumulation, while regular movement and exercise promote blood flow. Maintaining a low-sodium diet can also help to manage fluid retention. If you have swelling in your ankles that persists, or that is accompanied by pain, redness, or warmth, it is suggested that you schedule an appointment with a podiatrist for a proper diagnosis and treatment plan.
Swollen feet can be a sign of an underlying condition. If you have any concerns, contact one of our podiatrists of Complete Foot & Ankle Specialists, LLC. our doctors can provide the care you need to keep you pain-free and on your feet.
Swollen feet are a common ailment among pregnant women and people who stand or sit for extended periods. Aging may increase the possibility of swollen feet and patients who are obese often notice when their feet are swelling too. There may be medical reasons why swollen feet occur:
- Phlebitis - A condition that causes the veins to become inflamed and can also cause leg pain.
- Liver disease - This may lead to low blood levels of albumin which is a protein. This can cause fluid in the blood to pass into the tissues and several areas of the body can become swollen.
- Heart failure - When the heart doesn’t pump properly the blood that is normally pumped back to the heart can pool in the veins of the legs causing swollen feet.
- Kidney disease - One of the main functions of the kidneys is releasing excess fluid in the body. This type of condition can make it difficult for the kidneys to function properly, and as a result the feet may become swollen.
- Deep-vein thrombosis (DVT)- This is a serious condition where blood clots form in the veins of the legs. They can block the return of blood from the legs to the heart which may cause the feet to swell. It is important to be treated by a podiatrist if this condition is present.
Swollen feet can also be caused by bone and tendon conditions, including fractures, arthritis, and tendinitis. Additionally, there may be skin and toenail conditions and an infection may cause the feet to swell. Patients who take medicine to treat high blood pressure may be prone to getting swollen feet.
Many patients elevate their feet to help relieve the swelling and this is generally a temporary remedy. When a podiatrist is consulted the reason behind the swelling can be uncovered and subsequently treated.
If you have any questions please feel free to contact our offices located in Bellefontaine, OH and Springfield, OH . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Swelling of the Feet
There are many reasons why patients experience swelling of the feet. It is rather common and may be a side effect of pregnancy or from sitting and standing for most of the day. Gravity could also play a role in the development of swollen feet. It is known that the weight of blood volume in our bodies is exerted on the veins in the legs and feet. The veins may not work as efficiently during the aging process, and this could make the blood flow backward causing swollen feet. Relief may be found when obese patients lose weight, and it may help to engage in compression therapy by wearing compression socks, stockings, or athletic sleeves. This method can release pressure on the feet and ankles which may help to reduce existing swelling. There are patients who have controlled their swollen feet by implementing healthy lifestyle changes. These can consist of reducing salt intake, incorporating a gentle exercise regime into the daily routine, and drinking plenty of fresh water. Swollen feet may be a temporary condition that affects people who travel via airplane or automobile, so it is beneficial to walk as frequently as possible even though it can be difficult. Swelling of the feet can also be indicative of other health issues so it is important to pay attention to any type of chest pain, mental confusion, dizziness, or fever. If you consistently have swollen feet, it is strongly suggested that you consult with a podiatrist who can help determine the cause and how to effectively treat it.
What Can Cause Plantar Fasciitis?
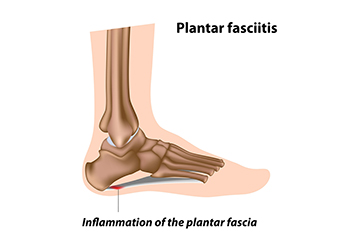
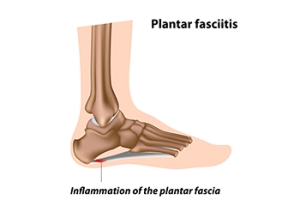
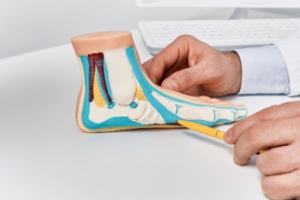
The plantar fascia is a thick band of tissue that connects the heel to the toes. Plantar fasciitis, an inflammation of this tissue, can stem from various biomechanical factors. Problems like an abnormal lower leg structure, limited ankle movement, and inward or outward heel or foot angles can strain the plantar fascia. These abnormalities can alter foot mechanics, leading to excessive tension and micro-tears in the fascia. Symptoms include sharp heel pain, especially after prolonged periods of standing or walking, which tends to improve with rest but worsens upon resuming activity. Early morning stiffness and tenderness in the heel or arch are also common. Addressing these biomechanical issues through proper footwear, orthotics, stretching exercises, and avoiding excessive strain on the feet can help to manage symptoms and prevent recurrence of this ailment. If you have been afflicted by plantar fasciitis, it is suggested that you confer with a podiatrist who can offer you various effective treatment methods.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact one of our podiatrists from Complete Foot & Ankle Specialists, LLC. our doctors can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our offices located in Bellefontaine, OH and Springfield, OH . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Plantar Fasciitis
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is the thick band of tissue that connects the heel bone to the toes. When this band of connective tissue becomes inflamed, plantar fasciitis occurs. Fortunately, this condition is treatable.
There are several factors that may put you at a greater risk for developing plantar fasciitis. One of the biggest factors is age; plantar fasciitis is common in those between the ages of 40 to 60. People who have jobs that require them to be on their feet are also likely to develop plantar fasciitis. This includes factory workers, teachers, and others who spend a large portion of their day walking around on hard surfaces. Another risk factor is obesity because excess weight can result in extra stress being placed on the plantar fascia.
People with plantar fasciitis often experience a stabbing pain in the heel area. This pain is usually at its worst in the morning, but can also be triggered by periods of standing or sitting. Plantar fasciitis may make it hard to run and walk. It may also make the foot feel stiff and sensitive, which consequently makes walking barefoot difficult.
Treatment for plantar fasciitis depends on the severity of the specific case of the condition. Ice massage applications may be used to reduce pain and inflammation. Physical therapy is often used to treat plantar fasciitis, and this may include stretching exercises. Another treatment option is anti-inflammatory medication, such as ibuprofen.
If you suspect that you have plantar fasciitis, meet with your podiatrist immediately. If left untreated, symptoms may lead to tearing and overstretching of the plantar fascia. The solution is early detection and treatment. Be sure to speak with your podiatrist if you are experiencing heel pain.
Managing Your Flat Feet
Flat feet, or fallen arches, occur when the arches of the feet collapse, causing the entire sole to touch the ground. While some individuals have flat feet from childhood, others may develop them later in life. A primary cause of flat feet is genetics. If your parents or grandparents had flat feet, there is a higher likelihood of inheriting the condition. Additionally, injuries or stress to the feet's tendons and ligaments or standing for long periods of time can lead to flat feet. Symptoms may include foot pain, swelling, and difficulty with movement. In severe cases, surgical intervention may be necessary to reconstruct the arches. To accurately diagnose the extent of flat feet and determine what the most effective treatment plan is, it is important to consult a podiatrist. They can provide expert assessment, recommend appropriate interventions like custom orthotics, and ensure ongoing management to alleviate symptoms and improve foot function. It is suggested that you schedule an appointment with a podiatrist for personalized care and relief from flat feet.
Flatfoot is a condition many people suffer from. If you have flat feet, contact one of our podiatrists from Complete Foot & Ankle Specialists, LLC. our doctors will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact our offices located in Bellefontaine, OH and Springfield, OH . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Flat Feet
Flatfoot is a foot condition in which the arch of the foot has either partially or totally dropped or has never developed. While it is common in babies and small children, it can become a problem for them in adulthood if the arch never forms. For adults, the development of flat feet can be brought upon by injury, as a result of pregnancy due to increased elasticity, or obesity. Those who have health concerns such as rheumatoid arthritis or diabetes may also be at greater risk for developing the condition.
If you suspect that you have flat feet, it is best to consult your podiatrist. Your foot doctor will examine the suspected foot and observe how it looks while you sit and stand. He or she may take an X-ray to determine how serious the condition is. Some common signs of flatfoot include toe drift, in which the toes and front part of the foot point outward, a short Achilles tendon, and a heel that tilts outwardly while the ankle tilts inward.
Once flatfoot has been diagnosed, your podiatrist may suggest one of several treatment options. Flat feet can be rigid, in which the feet appear to have no arch even when the person is not standing; or flexible, in which the person appears to have an arch while not standing, but once standing the arch disappears. Those with flexible flatfoot may be told to reduce any activities that cause pain and to avoid extended periods of walking or standing. Another suggestion may be weight loss, as excessive weight may be placing pressure on the arches
In few cases, if the condition is severe and all other methods have been exhausted surgery may be required. This is normally avoided, however, due to a lengthy recovery time and high cost.
What Does Diabetic Limb Salvage Mean?

Diabetic limb salvage is a medical approach focused on preventing amputations in patients with diabetes. Diabetes can lead to poor circulation and nerve damage, particularly in the lower extremities, increasing the risk of severe infections and ulcers. Limb salvage involves a comprehensive treatment plan aimed at healing these ulcers, improving blood flow, and managing infections. This multidisciplinary approach includes wound care, surgical interventions, and lifestyle modifications to control blood sugar levels and enhance overall foot health. The goal is to preserve the patient's limbs, improve quality of life, and prevent the devastating impact of amputation. Timely intervention and continuous care are essential to the success of diabetic limb salvage, emphasizing the importance of regular medical check-ups and early treatment of any foot issues in diabetic patients. If you have diabetes, it is strongly suggested that you are under the care of a podiatrist who can evaluate your condition, and educate you about methods that may help to avoid amputation.
Diabetic Limb Salvage
Diabetic limb salvage can be an effective way in preventing the need for limb amputation. If you have a foot ulcer and diabetes, consult with one of our podiatrists from Complete Foot & Ankle Specialists, LLC. our doctors will assess your condition and provide you with quality foot and ankle treatment.
What Is Diabetic Limb Salvage?
Diabetic limb salvage is the attempt of saving a limb, such as the foot, that has an infected ulcer, from amputation. Podiatrists also try to make sure that there is enough function in the foot after the salvage that it is still usable. Those with diabetes experience poor blood circulation, which prevents proper healing of an ulcer. If the ulcer is left uncheck, it could become infected, which could result in the need for amputation.
Diabetes is the number one cause of non-traumatic amputations in the United States. Amputation has been found to lead to higher mortality rates. This translates into higher healthcare costs, and a reduced quality of life and mobility for amputees. Podiatrists have attempted to increase the prevalence of limb salvage in an attempt to solve these issues.
Diagnosis and Treatment
Limb salvage teams have grown in recent years that utilize a number of different treatments to save the infected limb. This includes podiatrists that specialize in wound care, rehabilitation, orthotics, and surgery. Through a combination of these methods, limb salvage has been found to be an effective treatment for infected limbs, and as an alternative to amputation. Podiatrists will first evaluate the potential for limb salvage and determine if the limb can be saved or must be amputated.
If you have any questions, please feel free to contact our offices located in Bellefontaine, OH and Springfield, OH . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Diabetic Limb Salvage
Limb salvage is a procedure that involves saving a lower extremity from amputation. In podiatry, limb amputation often occurs as a result of diabetes. The fundamental goal of limb salvage is to restore and maintain stability and movement of the affected lower extremity.
The procedure typically involves removing the diseased tissue and a small portion of the surrounding healthy tissue, as well as the removal of any affected bone if necessary. If bone is removed it is then replaced with prostheses, or synthetic metal rods or plates, or grafts from either the patient’s body or a donor. Limb salvage is typically the preferred choice of procedure over amputation, as the procedure preserves both the patient’s appearance and allows for the greatest possible degree of function in the affected limb.
Upon diagnosis and determining that limb salvage is the appropriate treatment, the podiatrist may enlist the help of a physical and/or occupational therapist to prepare the patient for surgery by introducing various muscle-strengthening, walking, and range of motion exercises. Such exercises may be continued as rehabilitation post-procedure.